School-based health centers (SBHCs) cannot be sustainable on grant funds alone. Billing and reimbursement for services provided by the SBHC must be addressed during the planning process and included in the SBHC narrative business plan and pro-forma financial statement. In billing and reimbursement language, the patient is the first party, the provider is the second party, and insurers are the third parties. Major payment sources include third party funding from private insurance, Medicaid, children’s health insurance program (CHIP); second party, provider discounted rates; and patient self-pay from direct patient billing. Third party reimbursement occurs when an SBHC receives payment from a source other than the patient or a provider discount for services provided to the patient by a provider.
Private Insurance
Ask your school district collaborating partner for data on the percentage of students enrolled in the school where your SBHC is located who have private insurance, and with which private insurance carriers (i.e. Blue Cross Blue Shield, UnitedHealthcare, Aetna, Kaiser Permanente, Cigna, etc.). The SBHC and /or its primary care, behavioral health, oral health, and /or vision providers should seek and secure provider contracts with the prevailing private insurance carriers covering the students in the school(s) you serve.
Medicaid and CHIP
Medicaid and CHIP are means tested entitlement programs financed by states, some localities, and the federal government. These programs are designed and administered by states under federal statute. State governments determine which services beyond the minimum federal program requirements will be covered, how they will be covered, and at what reimbursement rate. Over the last decade, many states have combined eligibility and other processes such as billing for Medicaid and CHIP programs. In order for an SBHC and/or provider to bill and receive reimbursement from Medicaid/CHIP, they must meet required qualifications, be credentialed as an approved Medicaid provider, and obtain a Medicaid/CHIP provider number. The percentage of students eligible for free and reduced lunch at their school is a good indicator of the percentage of students eligible for Medicaid/CHIP. Most students served by SBHCs meet Medicaid/CHIP eligibility requirements, but they must be enrolled in Medicaid/CHIP in order for the services they receive to be billed to and reimbursed by either of these third party payers. SBHCs should facilitate Medicaid and CHIP outreach and enrollment for eligible patients and their families who are not currently enrolled, either onsite or by referring them to a nearby outreach and enrollment site.
FEE-FOR-SERVICE
Some Medicaid enrollees are served through a fee-for-service delivery system where health care providers are paid for each service (like an office visit, test or procedure). An enrollee may go to any Medicaid enrolled provider who meets program participation requirements. Providers accepting Medicaid patients accept Medicaid payments as payment in full; payments are made directly to providers. Each state determines their payment rates and publishes them online annually in a physician payment schedule. States describe payment methodologies for mandatory and optional Medicaid services in their Medicaid State plan. The Centers for Medicare and Medicaid Services (CMS) review all state plan amendments to make sure reimbursement methodologies are consistent with federal statutes and regulations. Payment rates are often updated based on specific trending factors, such as the Medicare Economic Index or a Medicaid-specific trend factor that uses a state-determined inflation adjustment rate. The methodologies for service rates are described in each state’s Medicaid plan.
MANAGED CARE
States have traditionally provided benefits to Medicaid patients by using a fee-for-service system. However, in the past 15 years, states have increasingly implemented a managed care delivery system for Medicaid benefits. In a managed care delivery system, individuals receive most or all of their Medicaid services from an organization under contract with the state. Nearly 50 million people receive benefits through some form of managed care, either on a voluntary or mandatory basis. States can allow Medicaid eligible beneficiaries to voluntarily enroll in a managed care program, but more commonly, states require people to enroll in a managed care program. When states implement a managed care program, they can use any one of the following types of entities:
- Managed Care Organizations (MCOs) – like HMOs, these companies agree to provide most Medicaid benefits to people in exchange for a monthly payment from the state.
- Limited benefit plans – these companies may look like HMOs but only provide one or two Medicaid benefits (like mental health or dental services).
- Primary Care Case Managers – these individual providers (or groups of providers) agree to act as an individual’s primary care provider, and receive a small monthly payment for helping to coordinate referrals and other medical services.
Self-Pay
If a patient has no coverage from a third party payer, they are considered self-pay and required to pay the sponsoring organization’s fee for services. School-based health centers, especially those sponsored by federally-qualified health centers and/or local health departments, will adjust their fees using a discounted fee scale, also known as a sliding fee scale. Discounted fee scales are based on federal poverty levels and percentages of fees due are discounted based on the patient’s income and family size. A fee schedule can slide to zero.
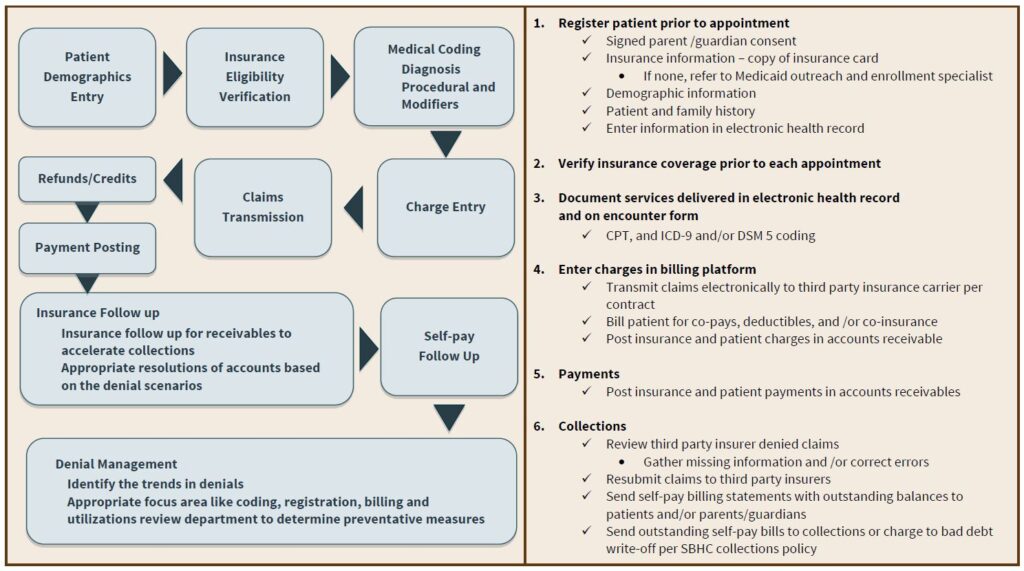
SBHC Billing and Collections
LIFE CYCLE OF A BILL IN AN SBHC