The Back-to-School Fall Learning Series
September 30 – October 30, 2025
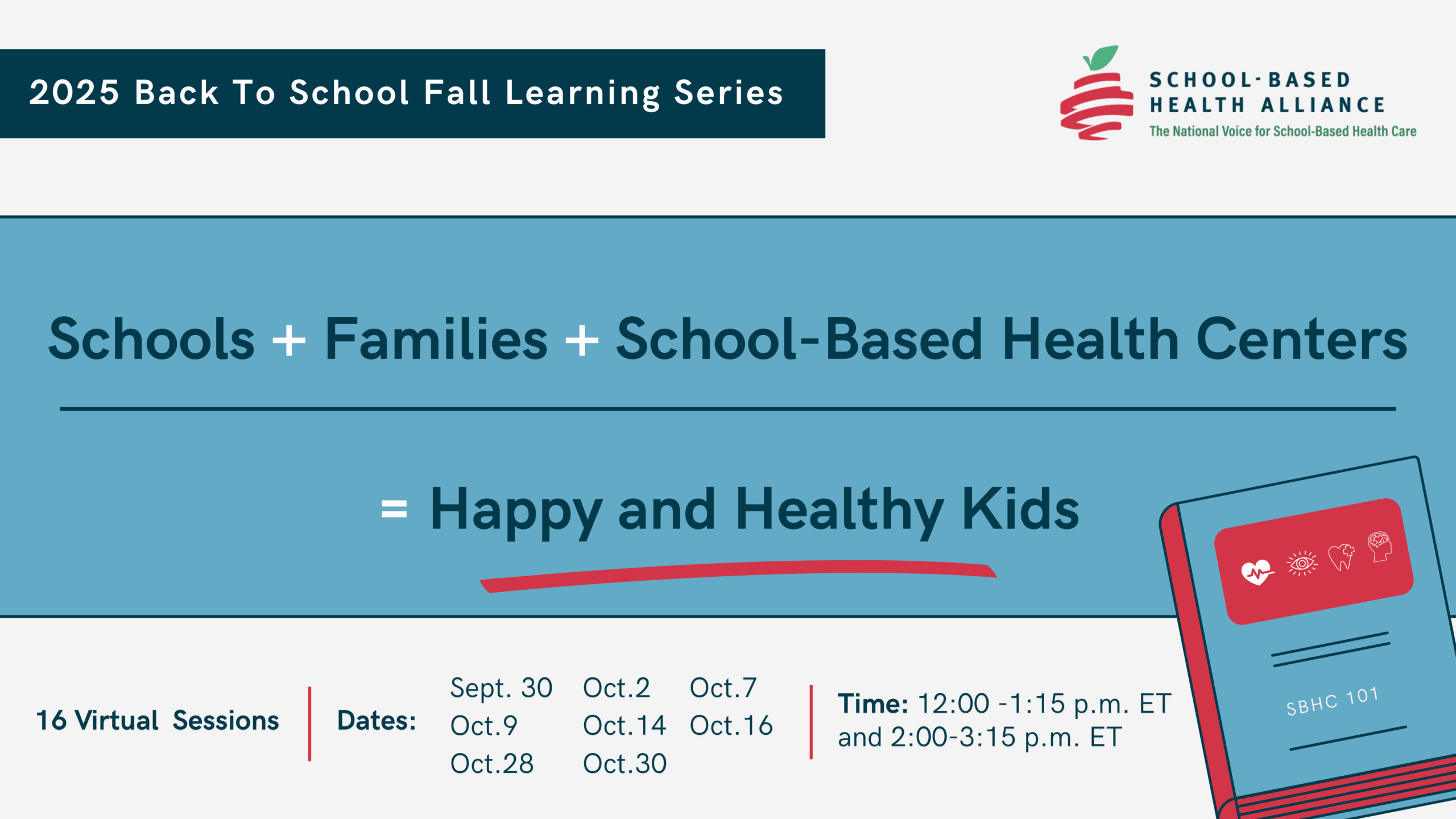
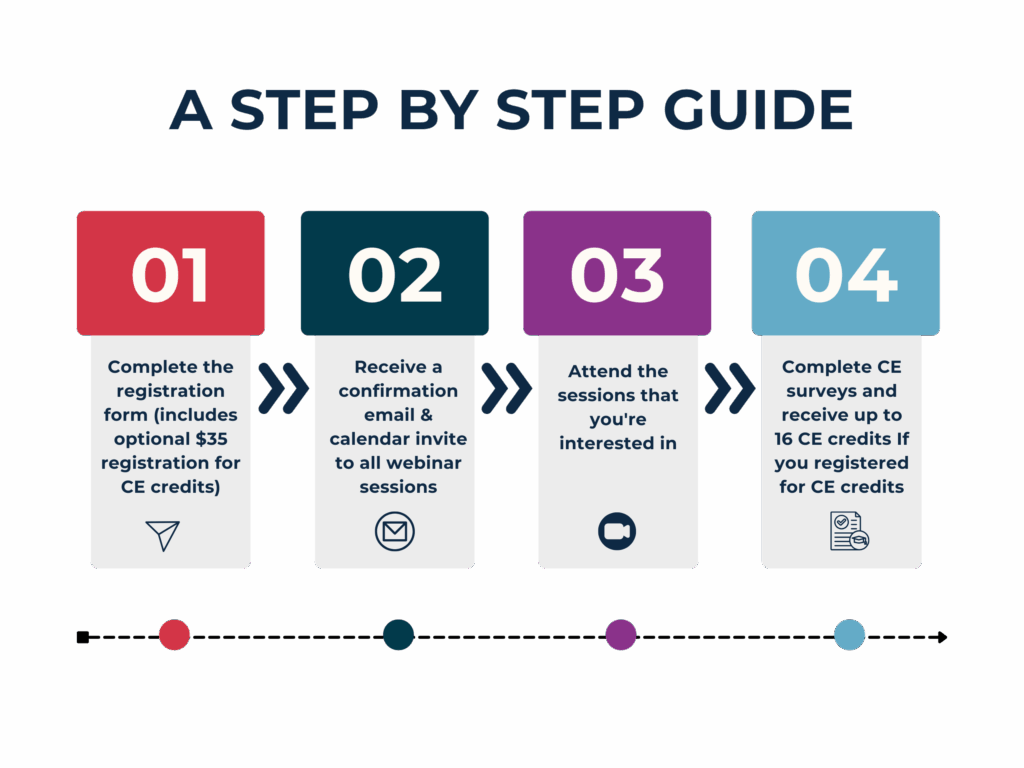
The School-Based Health Alliance will hold a FREE, virtual learning series exploring how schools, families, and school-based health centers can work together to support happy and healthy kids. This 16-session series will offer valuable insights and practical strategies to strengthen student well-being.
While the series is free, attendees can earn continuing education credits (CE Credits) for a fee of $35. Webinar recordings will not be available once the learning series ends.
Dates
Time
Sept.30 | Oct. 2 | Oct. 7 | Oct. 9 | Oct. 14 | Oct.28 | Oct. 30
12:00 – 1:15 p.m. ET and 2:00 – 3:15 p.m. ET
The sessions information
+
Series A
12:00–1:15 PM ET
Health-E You: Designing and Implementing a Youth-Centered App to Support Sexual Health
Speaker: Kathleen Tebb, PhD
Health-E You/Salud iTuTM is an interactive, individually tailored web-based mobile health application that has been proven effective in facilitating patient-centered sexual and reproductive health (SRH) care, resulting in significant increases in contraceptive use among sexually active adolescents seeking care at school-based health centers. In Phase I of this workshop, we will review the importance of SRH care in young people’s health and development, share the youth engagement approaches used in the development of the Health-E You app, and findings from the randomized control trial and the current dissemination and implementation study. In Phase II, we will introduce our current work to expand Health-E You to young people of all sexes and genders. This session equips participants with strategies to create more inclusive, relevant, and impactful interventions tailored to youth needs.
Change Management: Redesign of SBHC Infrastructure to Achieve Long-Term Success & Sustainability
Speaker: Stephanie Ramirez, MHA
In August 2024, Legacy School-Based Health Clinics (SBHC) experienced significant changes in staffing, telemedicine care delivery, and productivity expectations to reduce negative financial impact for long-term success and sustainability. Legacy is the largest FQHC SBHC in the nation, with 37 schools providing behavioral health (BH) and pediatric services to communities in vulnerable areas across the greater Houston area. As a result of changes, SBHC nurse clinicians were realigned from 37 to 17, transformed telemedicine capability through the introduction and use of devices, implemented the Performance Action Initiative (PAI) for BH, and weekly productivity reporting for pediatrics. We will discuss the method for determining minimum daily patient volume expectations, the impact of increased volume expectations, changes in clinical assignment, and how changes were managed for improved results through data collection and reporting.
SBHCs HELP: School-Based Health Centers Address Health Equity for LGBTQ+ Patients
Speaker: Mary Ramos, MD, MPH
This workshop describes a four-year community-engaged implementation science study (R01NR021019) that aims to improve the experiences of LGBTQ+ students receiving care in school-based health centers (SBHCs). Through this newly initiated study, 24 participating SBHCs in New Mexico receive support in implementing five changes to delivery settings that are likely to improve SBHC structural competency in addressing upstream factors (e.g., stigma, discrimination, fragmented treatment, and other social determinants of health) that negatively impact the health and health equity of LGBTQ+ youth. These five changes include fundamental things such as having policies in place to prevent discrimination, creating welcoming SBHC environments, training for providers and staff in best practices, clinical workforce development, and using data about the sexualities and gender identities of patients to improve care.
This workshop will cover the need for and importance of implementation science studies such as this one, theoretical foundations, innovative methodology, and preliminary findings after the first full academic year of implementation.
Collaborative Nutrition Counseling for Adolescents in School-Based Health Centers
Speaker: Natalie Nation, MPH, RD, LD
Effective nutrition care in SBHCs requires dynamic collaboration between dietitians and other healthcare providers. This presentation will explore techniques for fostering collaborative teamwork, ensuring that nutrition counseling is fully integrated into the broader scope of clinic services. The presenter will discuss the benefits of integrating nutrition counseling into SBHCs and share practical advice and case studies of successful communication and collaboration between dietitians and other clinic providers to improve student health outcomes. Adolescent-centered care requires healthcare providers to recognize the rapidly shifting social and emotional development teens face alongside the physical changes that occur during puberty. By integrating nutrition counseling into SBHCs, all providers can play a critical role in shaping the long-term health trajectories of young people. Participants will learn in this session evidence-based strategies and advocacy tools to enhance or expand nutrition services in their own settings, fostering a holistic and equitable approach to student health.
Ask, Act, Prevent: Implementing the ASQ Suicide Screening Toolkit for Early Intervention
Speakers: Florencia Kantt, MSN, CPNP-PC, Enyo Dzara, DNP, MSN
With rising mental health challenges among adolescents, school-based health centers (SBHCs) have a unique role in identifying and addressing suicide risk in young people. The Ask Suicide-Screening Questions (ASQ) Toolkit provides a simple yet powerful tool for early detection of suicide risk, equipping providers to initiate life-saving conversations and connect at-risk students with the care they need. This session will introduce participants to the ASQ toolkit, emphasizing practical steps for screening, referral, and follow-up that are tailored to the school setting. By the end of this session, providers will feel prepared to adopt the ASQ toolkit confidently, fostering a proactive approach to suicide prevention in schools and promoting a culture of mental health awareness and support.
Informatics Resources for Social Determinants of Health in School-Based Health Centers
Speaker: Vera Borkowski, PhD, APRN, FNP-C
School-based health centers are ideally placed to facilitate identification of social risk factors and social needs. It is unclear whether school-based health center providers consider social determinants of health (SDoH) information as possibly related to a lack of SDoH knowledge or data availability. We sought to understand the awareness of SDoH information and assessment of social risk factors in school-based care, especially with patients at risk for asthma exacerbations. This presentation reviews the methods and findings of a predoctoral dissertation focused on understanding the information-gathering behaviors for social risk screening in school-based health centers. Using an exploratory sequential design, we collected qualitative data from virtual focus groups using a semi-structured interview and performed a group concept mapping study where we interviewed families/caregivers, school nurses, school staff, and school-based health center providers. We also developed an informatics resource for SDoH and social risk factors for asthma exacerbations that can be used in school-based health centers. We completed data collection and have a description of providers’ demographics, and school-based health center factors. We used the focus group self-reported information on how providers access social screening data and factors that are feasible to address in SBHC. Next, we used human-centered design to develop an informatics resource and performed usability testing and interviews for feedback from Connecticut SBHC providers. By presenting SDoH in a useful and usable way, increased social risk screening and tailored social needs assessment can be performed, leading to preventative education and treatment to decrease exacerbations, health inequities, and medical expenditures. The potential clinical implication is our long-term goal is to integrate SDoH data into care delivery to promote early, targeted screening and assessment in the management of many childhood illnesses.
Strengthening Student Health for Primary Care
Speaker: Veda Johnson, MD
This session highlights the critical role of SBHCs in delivering primary care to students. Participants will explore strategies for enhancing care delivery, addressing barriers, and promoting comprehensive, student-centered health services within the school setting. The discussion will also examine how SBHCs can strengthen preventive care, manage chronic conditions, and support whole-child wellness. Attendees will leave with practical insights and examples that can be adapted to diverse school and community contexts.
“I bought it at the Vape Shop”: Misunderstood substances and adolescent dependence
Speaker: Steve North, MD, MPH
Over 31% of 12th graders reported using an illicit substance in the prior 12 months according to the Monitoring the Future Study; however <1% of 12th graders reported using an opiate. During the same time frame, approximately 23% and 25%report vaping and being drunk, respectively, substances that are readily available to adolescents in most communities. A significant portion of this illicit substance use is fueled by substances available at gas stations, convenience stores, and vape shops. They are frequently marketed to help people relax or have more energy, and therefore, adolescents view them as safe despite the high potential for adverse events or dependency. This workshop will introduce harm reduction as an evidence-based approach to caring for people who use illicit substances and frame substance use disorders as chronic diseases. Through a series of cases, current and emerging best practices for caring for people who use drugs will be explored, including harm reduction, medication, and behavioral health interventions.
Series B
2:00–3:15 PM ET
Boosting School Immunization Compliance: Practical Strategies for Effectively Engaging Schools and Families
Speaker: Diana Bruce, MPA
Ensuring immunization compliance in schools is a complex but critical responsibility that requires a comprehensive, collaborative approach. This session will teach participants how to evaluate and improve their school’s immunization processes using a real-world case study that combines insights from educators, families, and healthcare professionals. Recovering from pandemic-era, low-immunization rates, it’s more important than ever to ensure schools have robust, effective processes in place. By focusing on teamwork, data management, family engagement, and accountability, schools can streamline their immunization efforts and foster a healthier community. We’ll explore how to maximize the use of available resources, such as district health databases and immunization tracking systems, and a robust and collaborative team—with Administrators, nurses, and IPOC teams working in sync (and how it dramatically improves your school’s immunization efforts). Next, we’ll dive into the key to success – the art of effective family engagement and data management. We’ll show you how to communicate persistently and creatively with families, ensuring they understand the importance of immunizations, have compliance deadlines in mind, and can navigate around competing family priorities and barriers to care while fostering a positive home and school relationship. We’ll analyze techniques to prioritize regular data entry and track student immunization status efficiently. Along the way, we’ll discuss the importance of recognizing progress, celebrating large and small wins, keeping your team motivated, and building momentum. Finally, we’ll cover how to enforce exclusion policies with empathy and transparency, ensuring the safety and well-being of your school.
By the end of the session, you’ll be equipped with a proven set of strategies to improve immunization compliance, enhance teamwork, and build stronger connections with families—all while ensuring your school remains compliant and healthy.
“Future in Focus: A Discussion with the SBHA Youth Advisory Council”
Speakers: Ketan Tamirisa and Kauree Bennett
“Future in Focus: A Discussion with the SBHA Youth Advisory Council” will bring together members of the School-Based Health Alliance’s Youth Advisory Council (YAC) for a dynamic conversation about the future of school-based health care. During this session, our youth leaders will share their perspectives on current challenges, opportunities, and priorities for improving student health and well-being. Participants will hear directly from young people about what matters most to them and how their voices can shape programs, policies, and practices.
Clinical Updates in the Care of Newly Arrived Immigrant Students
Speaker: Lauren Jen, MD
Newly arrived immigrant children require specialized medical care. The content of this workshop will instruct on the best-practice guidelines for the care of newly arrived immigrant children and adolescents. This includes medical considerations, specialized elements of the history, physical, and laboratory testing. We will discuss the evaluation of international immunization records and review the catch-up schedule. Additionally, this workshop will provide special considerations for refugee and asylum-seeking families. We will also evaluate the behavioral health and reproductive health needs of these students.
From Vision to Action: Implementing School-Based Oral Health
Speaker: Tamara Baker, MPH
This presentation, by the School-Based Health Alliance of Arkansas (SBHAAR) and Virginia Health Catalyst (Catalyst), will guide participants through the initial stages of implementing a successful school-based oral health program (SBOHP). Grounded in a framework developed by Catalyst, this interactive session introduces “Building Common Language” and “Building a Common, Specific Model”—the first two components of a 10-step plan to support Arkansas schools in establishing robust oral health services. By the session’s conclusion, participants will have a clear understanding of how to lay the groundwork for a sustainable SBOHP. This includes mastering best practices for program setup and developing a tailored, replicable model for enhancing student health and academic success.
Patient Navigators as the Core of School-Based Health Center Staffing: Strengthening Community Engagement and Student Connections
Speaker: Anjulle Morales, BSN
This workshop will highlight how employing Patient Navigators in school-based health centers can help bridge these gaps by facilitating community engagement, delivering culturally competent care, and ensuring that the students who need it most receive the support they deserve. The workshop will be structured in four key sections: Overview of the Role of Patient Navigators: This section will cover the day-to-day responsibilities of a school-based Patient Navigator, highlighting how they form connections between students, families, and healthcare services. Staffing Model for Maximizing Access and Establishing Presence: We will discuss the staffing model that integrates Patient Navigators into school-based health centers, ensuring that even when direct healthcare services are not available, there is always a trusted point of contact on campus that keeps students connected to our services. Training for Navigators: This section will highlight the training that prepares individuals for their role as school-based Patient Navigators, meeting the needs of students from diverse backgrounds and addressing the Social Determinants of Health. Engagement Strategies for Pacific Islander and Hispanic Communities. A core part of the workshop will highlight effective strategies for engaging Pacific Islander and Hispanic students and their families. We will discuss how patient navigators build strong relationships with these communities by providing culturally sensitive support, proactive outreach, and partnering with local organizations that service these communities.
Home Sweet Home – Creating a dental home in an SBHC through TeleORALHealth
Speaker: Dani Ford, MHA, RDH
This session is intended to broaden the scope of thought behind what constitutes a “dental home” for a patient. No longer does it have to be a brick-and-mortar office, owned by a dentist. School-Based Health Centers (SBHCs) are prime locations for a virtual dental home through synchronous and asynchronous teledentistry utilizing a Registered Dental Hygienist (RDH) as the primary in-person provider. This course will address the successful pilot and care model completed within the school-based oral Health department within Denver Health Pediatrics at Denver Public Schools, and the TeleORALHealth program occurring on the Western Slope of Colorado, facilitated by their Regional Oral Health Specialist. This allows patients to keep the SBHC as their primary healthcare home and receive oral healthcare when and how it is convenient for them. It encourages both the hygienists and dentists to practice at their highest scope, increases access to care, and minimizes unnecessary dental visits. This course will also address some of the varying scopes of practice by state, a brief legislative background on teledentistry, and the equipment needed to start a clinic.
Celebrating Neurodiversity and Supporting Neurodivergent Students in School-Based Health
Speaker: Caitlin Rossman, LMSW
The neurodiversity movement has been gaining traction in the mental health and education fields in recent years. However, there is still a lack of understanding of neurodivergent populations and a lack of appreciation for these students. This workshop will go beyond accepting neurodivergent individuals and will focus on celebrating them. We will explore concepts of neurodiversity, types of neurodivergent individuals, including autism, ADHD, OCD, and sensory processing differences, and how to best support these students. The focus of this workshop is to gain a better understanding of how these students function in school, and to reframe what schools, families, and medical professionals often see as “problem behaviors.” We will look at what is driving these behaviors and how the world and our schools are not set up to support neurodivergent students best. This workshop will help participants understand how to be neurodiversity-affirming, push against ableism in their health centers and schools, and advocate for these students. We will explore the specific challenges these students face in schools and how clinicians can support them in their individual work with these students, as well as working with school staff to support them in their classrooms. Participants will be able to go back to their school-based health centers and their schools, prepared to work with neurodivergent students, to provide psychoeducation to families and school staff about neurodiversity, and to advocate for the needs of these students and for more understanding, acceptance, and celebration of neurodiversity. They will specifically be able to explain concepts of neurodiversity, neurodivergence, and the neurodiversity movement, to show how to implement a neurodiversity-affirming approach, to identify common behavioral concerns for these students, to advocate for new strategies to work with these students, and to implement research and evidence-based practices in their own work with these students.
Encuentros: Grupos de apoyo emocional dirigidos por pares para jóvenes de secundaria (Spanish Only)
Este taller mostrará cómo, con el apoyo del personal de Identity en los Centros de Salud y Bienestar escolares del condado de Montgomery, Maryland, los jóvenes latinos y otros jóvenes históricamente desatendidos están sirviendo como agentes de cambio al ayudar a sus pares a manejar emociones difíciles relacionadas con la inmigración, la separación familiar y otras experiencias traumáticas.
Dirigido por el personal de Identity y los líderes de pares jóvenes, el taller explorará cómo, en respuesta a la actual crisis de salud mental juvenil, el programa no clínico Encuentros de Identity está capacitando a los participantes anteriores paraque faciliten conjuntamente grupos de apoyo emocional basados en evidencia donde puedan compartir recursos y estrategias para manejar emociones difíciles y hacer frente a los desafíos de salud mental.
En la Parte 1, el personal de Identity y los líderes de pares jóvenes demostrarán el programa en acción al dirigir una sesión abreviada de Encuentros. Los participantes tendrán la oportunidad de compartir sus propias historias y experiencias y aprender de las de los demás. Los facilitadores utilizarán la técnica del Diálogo en círculo, una forma de discusión estructurada en la que los participantes tienen la oportunidad de compartir sus propias historias y experiencias y aprender de las de los demás.
La segunda parte consistirá en una presentación que describirá la evolución del programa y el plan del estudio de impacto de Encuentros. El personal de Identity presentará datos de impacto de los socios de evaluación de la Facultad de Salud Pública de la Universidad de Maryland y explicará cómo el programa se ha mejorado continuamente en respuesta a las encuestas de los participantes y los grupos focales. Basándose en sus propias experiencias, los líderes de pares jóvenes describirán su recorrido desde participantes hasta cofacilitadores, mostrando cómo Encuentros ofrece un espacio restaurador donde los jóvenes pueden sanar compartiendo y escuchando las historias de los demás. Finalmente, se abrirá el espacio para cualquier pregunta del publico que haya surgido durante la presentación o la sesión grupal interactiva de Encuentros.